Q. What is DITI?
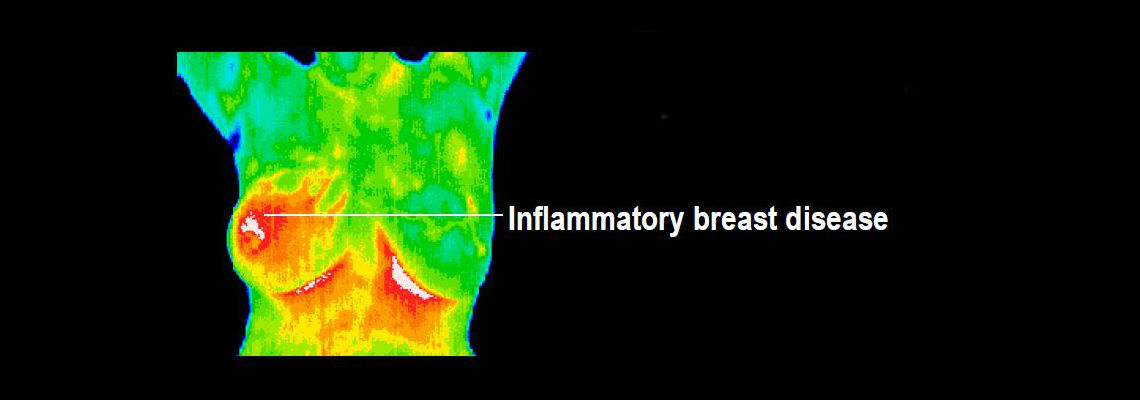
A. DITI or ‘Digital Infrared Thermal Imaging” is an imaging technique for measuring and displaying body temperature. It is a key diagnostic tool in the detection of disease, injury and infection. There is a high degree of thermal symmetry in a normal healthy body. Subtle abnormal temperature asymmetries can be easily identified that may be attributed to pathology or dysfunction. DITI relies on the principal that all objects at a temperature above 0 ° K (absolute zero) radiate infrared energy. The amount of radiation emitted is a function of the body’s physiology. Our DITI camera captures and records this energy and converts it to a digital image called a thermogram that is saved for analysis and archiving.
Q. Do I need my doctor’s referral?
A. No, Gaston Thermal Imaging, Inc. sees patients who are both self and physician referred.
Q. How do I prepare for my thermographic scan?
Preparing for your scan is simple, but crucial to the accuracy of the results. Do not have any physical therapy, electromyography, or chiropractic work the same day as your thermography appointment. Do not smoke or participate in vigorous exercise 2 hours before the test. Do not use any lotions, liniments or creams the day of your scan. Avoid strong sunlight exposure the day of your appointment. Please see our Exam Procedure page for more details.
Q. How long does the procedure take?
A. The scan itself take only 15 to 30 images depending on whether or you are having a single region of interest scan or a whole body scan performed. For more details please visit our Exam Procedure page.
Q. Why do I need to come back in three months for another breast study?
A. The most accurate result we can produce is change over time. Before we can start to evaluate any changes, we need to establish an accurate and stable baseline for you. This baseline represents your unique thermal fingerprint, which will only be altered by developing pathology. A baseline cannot be established with only one study, as we would have no way of knowing if this is your normal pattern or if it is actually changing at the time of the first exam. By comparing two studies three months apart we are able to judge if your breast physiology is stable and suitable to be used as your normal baseline and safe for continued annual screening.
The reason a three-month interval is used relates to the period of time it takes for blood vessels to show change. A period of time less than three months may miss significant change while a period of time much more than three months can miss significant change that may have already taken place. There is NO substitute for establishing an accurate baseline. A single study cannot do this.
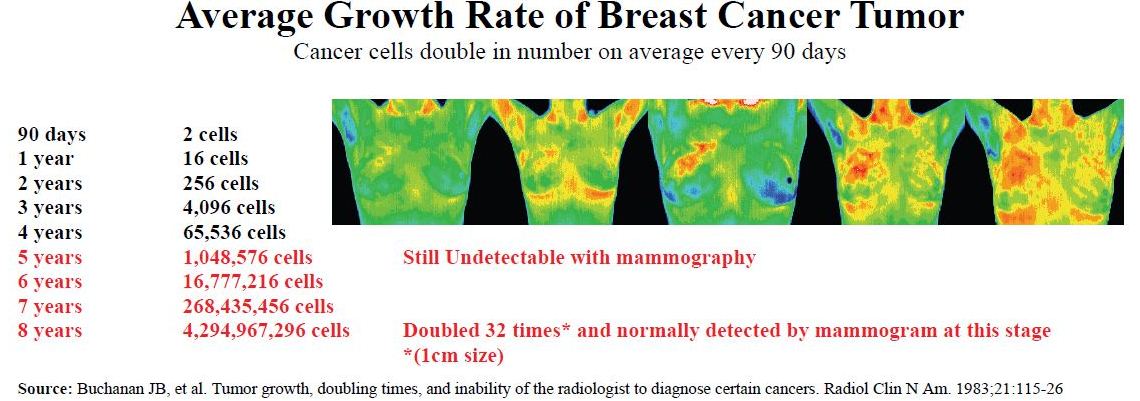
Q. Is a thermal scan different than a mammogram or ultrasound? Yes. Unlike mammography and ultrasound, Digital Infrared Thermal Imaging (DITI) is a test of physiology. It detects and records the infrared heat radiating from the surface of the body. It can help in early detection and monitoring of abnormal physiology and the establishment of risk factors for the development or existence of cancer. Mammography and ultrasound are tests of anatomy. They look at structure. When a tumor has grown to a size that is large enough and dense enough to block an x-ray beam (mammography) or sound wave (ultrasound), it produces an image that can be detected by a trained radiologist. A mammogram, ultrasound, or DITI cannot diagnose cancer. This is possible only through a biopsy. When DITI, mammograms, ultrasounds, and clinical exams are used together, the best possible evaluation of breast health can be made.
Q. Is thermal imaging a replacement for mammography or ultrasound? DITI should be viewed as a complimentary, not competitive, tool to mammography and ultrasound. DITI has the ability to identify patients at the highest level of risk and actually increase the effective usage of mammograms and ultrasounds. Research confirms that DITI, when used with mammography, can improve the sensitivity of breast cancer detection. The ultimate choice should be made on an individual basis with regard to clinical history, personal circumstances, and medical advice.
Q. If I have a suspicious mammogram or breast lump should I have a thermal scan? Yes. The information provided by a thermography study can contribute useful additional information which ultimately helps your doctor with case management decisions. It is also instrumental in the progress of any treatment protocol.
Q. I hear from some people that you need to “cold stress” the patient. What is “cold stressing”? Do I really need to do it?
A. Cold stressing is a test to measure sympathetic function. It is a useful test for a number of conditions including RSD (CRPS). Protocols for breast screening with the med2000 system do not require routine cold stressing but it may be requested by a referring physician or reading Thermologist.
Q. Who certifies your Thermographers?
A. Thermography technicians are trained and certified by the American College of Clinical Thermology at Duke University. The American College of Clinical Thermology is an accredited medical association.
Q. Who reads the images and reports?
A. Images are sent to an interpretation service that employs medical doctors who are all board certified as Thermologists by the American College of Clinical Thermology at Duke University. These doctors have many years experience and are able to ask for second opinions whenever necessary.
Q. How quickly will I get my report back?
A. Reports are normally ready within 48 hours and are generally emailed to you, your referring physician, and/or the practitioner of your choice. Should you require a paper copy of your report or if you need your report within 24 hours you will be required to pay an additional fee.
Q. Insurance?
A. Gaston Thermal Imaging is not participating with any insurance companies. While the procedure itself is FDA approved, most insurance companies consider it investigational and will not pay for it. However, as this is a qualified medical procedure, you may use your HSA, HRA, FSA or Flex Benefits Card to render payment.
Q. How much does imaging cost?
A. Click here to see our fee schedule.
Q: I don’t want to have a mammogram. Can I just get thermograms instead?
A: Mammograms and thermograms each miss about 15-18% of breast cancers, but they tend to miss different ones. Mammograms tend to miss the faster growing cancers which fail to produce calcium deposits, while thermograms tend to miss the slower growing cancers which fail to produce robust blood vessel growth. Therefore, using these studies together along with a doctor’s examination and regular self examinations provides the greatest probability of early detection.